The retina is the thin layer of nerve tissue lining the back of the eye. The retina functions much like the film in a camera and transmits light signals to the brain. The central and most sensitive part of the retina is called the “macula”.
Epiretinal Membrane (ERM)
What is an epiretinal membrane or Macular Pucker?
An epiretinal membrane or macular pucker is a fine layer of scar tissue that may grow on the surface of the retina.
The epiretinal membrane often builds up slowly over time and may contract, causing wrinkling of the retinal surface, which may affect your vision and quality of life.
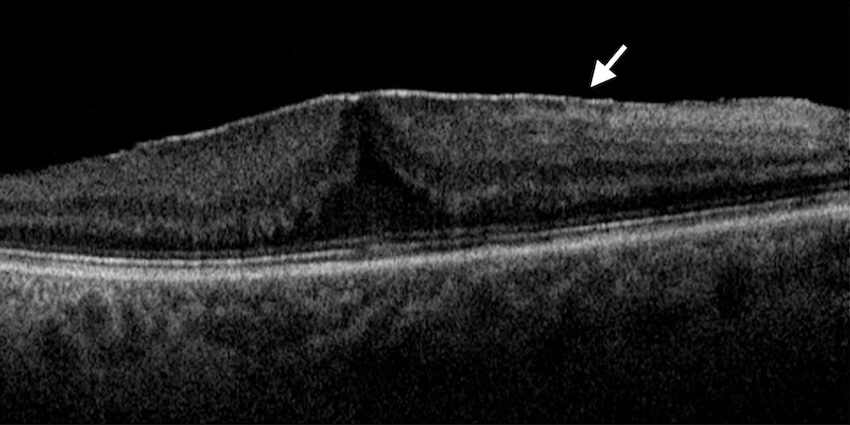
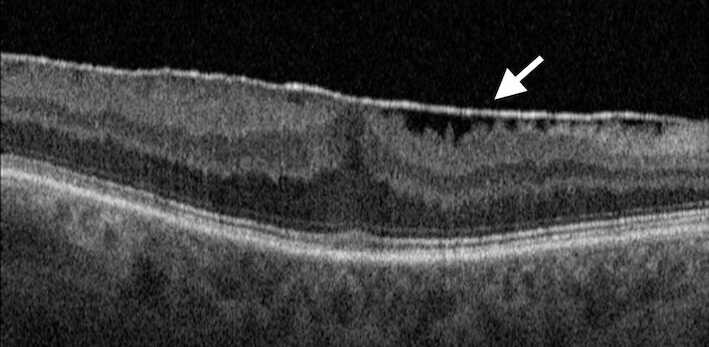
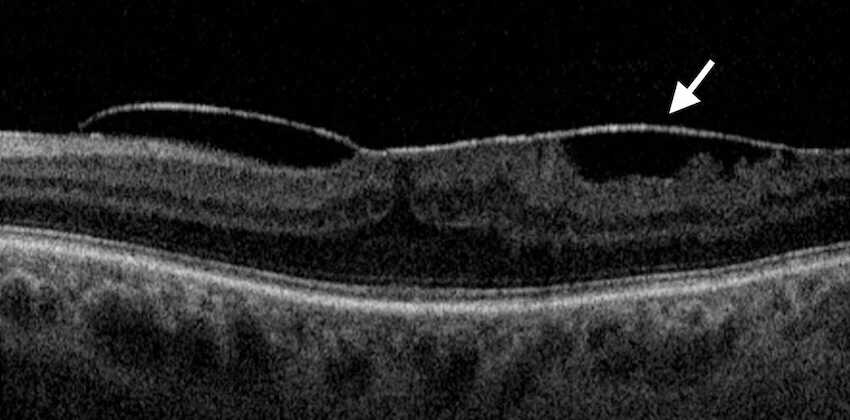
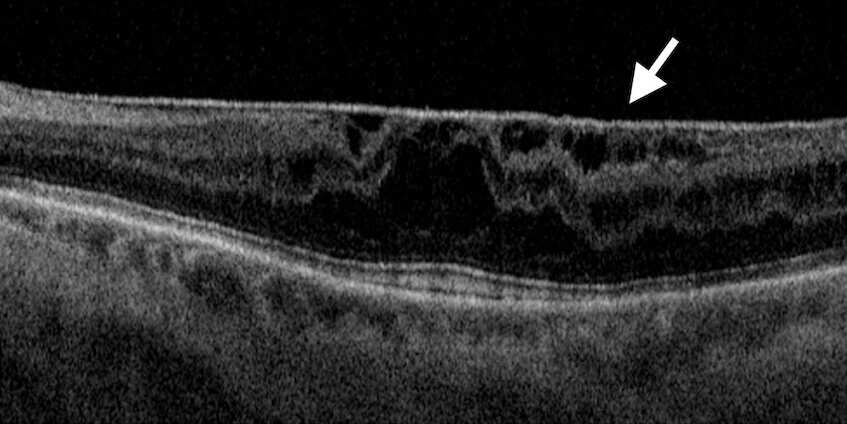
Different forms of epiretinal membrane
What are the symptoms?
The majority of cases are mild and have a limited impact on vision. However, in some people, the membrane may continue to grow slowly, causing further wrinkling of the retina, resulting in:
- Distortion of the image (straight lines appear wavy).
- Blurred vision particularly reading.
- Difference in the size of the image between both eyes.
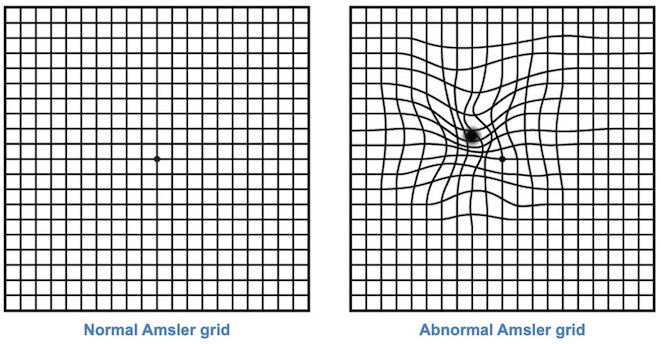
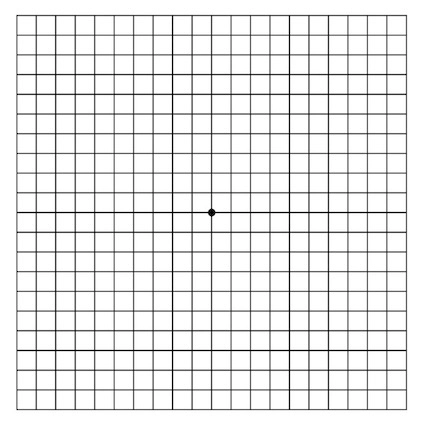
Once diagnosed with epiretinal membrane, it is important to regularly check your central vision with a certain grid called “Amsler grid”. This is a simple square containing a grid pattern and a dot in the middle. With an epiretinal membrane, you may notice the lines are wavy or distorted.
What causes it?
The exact cause of the epiretinal membrane is unknown. Normally, the eye is filled with a gel-like substance called “vitreous.” As we age, the vitreous shrinks and separates from the surface of the retina in a process called posterior vitreous detachment or separation. In some people, for an unknown cause, this may irritate the retinal surface, causing this scar tissue (membrane) to build up on the surface of the retina. These are often called the primary epiretinal membranes. This condition usually affects people over 60 years old.
However, sometimes the epiretinal membrane can form following previous retinal surgery, retinal laser treatment, eye injury, or inflammation, often called the secondary epiretinal membrane or macular pucker.
What is the treatment for epiretinal membrane?
In many patients, the membrane is minimal and has only a limited impact on vision; therefore, no treatment is needed. However, in some people, the membrane can be large, causing significant visual disturbance and making it difficult to carry out daily activities such as driving or reading. In such cases, the doctor may consider treatment, which is surgery to remove the membrane. Eye drops or stronger glasses will not help.
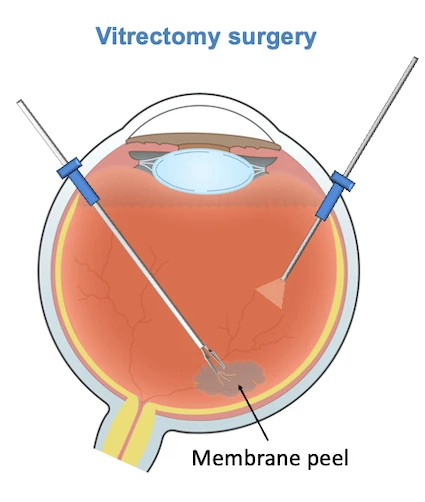
The surgery is called “vitrectomy” which involves removing the gel inside the eye using very small instruments. Then the membrane is peeled off the retina with the aid of fine micro-forceps.
Vitrectomy surgery is performed with the aid of local anaesthetic (small injection of anaesthetic solution around the eye) as day surgery. Your eye will be numbed and you will not feel any pain, although you may feel some pressure sensation during the surgery.
The surgery often takes about 45 minutes. The surgery is often combined with cataract surgery if you have a cataract.
If you have any queries about your suitability for epiretinal membrane surgery, you can fill out the form in the contact section.
Should I have the surgery for my epiretinal membrane?
Mr Ellabban will discuss with you in detail the surgery. The main reason to proceed with the surgery is to attempt to improve vision. If your symptoms are minimal and you are not aware of any visual problems, you might not need the surgery. However, if the distortion affects your ability to drive, read, or perform important tasks, you should consider having the surgery.
Will my vision recover completely after the surgery?
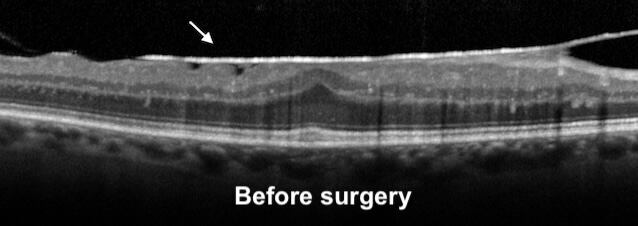
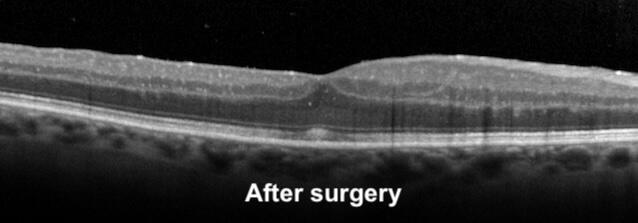
When the membrane is removed by surgery, you will usually notice an improvement in vision, particularly in the quality of vision. This usually takes a few weeks to months to reach the final improvement as the retina heals after the surgery. You will be followed with the aid of retinal scans to monitor the healing process and restoration of the retinal layers. Also, the central distortion and blurring will gradually improve after surgery; however, it will not be completely restored to normal.
What are the risks of the surgery?
Vitrectomy surgery has similar risks as other types of eye surgery. There is a small risk of complications such as:
- Infection
- Prolonged Inflammation
- Bleeding
- Retinal detachment
- Increased eye pressure
- Distortion or alteration of vision
What will happen afterwards?
Mr Ellabban will arrange a review after the surgery, to monitor the healing process of the retina. You will be monitored with the aid of retinal scans to assess the healing process and restoration of the retinal layers.
What I need to do after the surgery?
You are advised to follow the instructions you were given after the surgery by Mr Ellabban and the nursing team. In general, there are important points to follow, after retinal surgery:
- Put the drops as you were instructed.
- Avoid rubbing your eyes for 2 weeks.
- Avoid heavy lifting and straining for 2 weeks.
- Avoid getting soap or shampoo or any chemicals into your eye for 4 weeks.
- Avoid swimming for 12 weeks.
- You must not drive until you reach the minimum legal standard of vision.
- It is normal for the eye to appear red or uncomfortable for a few days after the surgery which will gradually get better over time.
What if I don’t have surgery?
As mentioned above, most cases of epiretinal membrane are mild, and no treatment is required. The surgery is only indicated for selected cases where the membrane is large or has a significant impact on vision while performing daily activities like reading or driving.
If no surgery is performed, the vision may remain the same, or continue to get worse as the epiretinal membrane can grow over time causing more distortion and blurring.
If you have any queries about your suitability for epiretinal membrane surgery, you can Request a Call Back by filling out the form in the contact section.
Waht is Amsler grid?
Amsler grid is a simple square containing a grid pattern and a dot in the middle. This grid can help to show if you have any problems with your central vision. It is recommended that all patients over 55 years of age regularly check their vision with the Amsler grid. This may help in the early detection of any problem in the central vision
How to use Amsler grid?
- Wear your reading glasses and hold the grid 12 to 15 inches (30 cm) in good light.
- Cover one eye.
- Look directly at the centre black dot with your uncovered eye and keep your eye focused on it.
- While looking directly at the centre dot, notice in your side vision if all grid lines look straight or if any lines or areas look blurry, wavy, dark or blank.
- Follow the same steps with the other eye.
- You can repeat this test at home every day.
If you notice any areas of the grid that appear darker, wavy, or blurry, contact your eye specialist right away to examine the back of the eye.